THANK YOU TO OUR SPONSORS
REGISTER TO ATTEND!
Join us for the University of Chicago’s Celiac Across the Lifespan Conference at the David Rubenstein Center in Chicago, Illinois, on Saturday, April 18th, 2026.
Attend this full-day symposium where top national and international experts will share the latest breakthroughs in celiac disease care and science. The agenda delivers high-impact, clinically relevant, and research-focused content covering advanced diagnostic protocols, screening and risk assessment, best practices for lifelong patient management and transitioning care, strategies for optimizing dietary adherence, and treating refractory celiac disease.
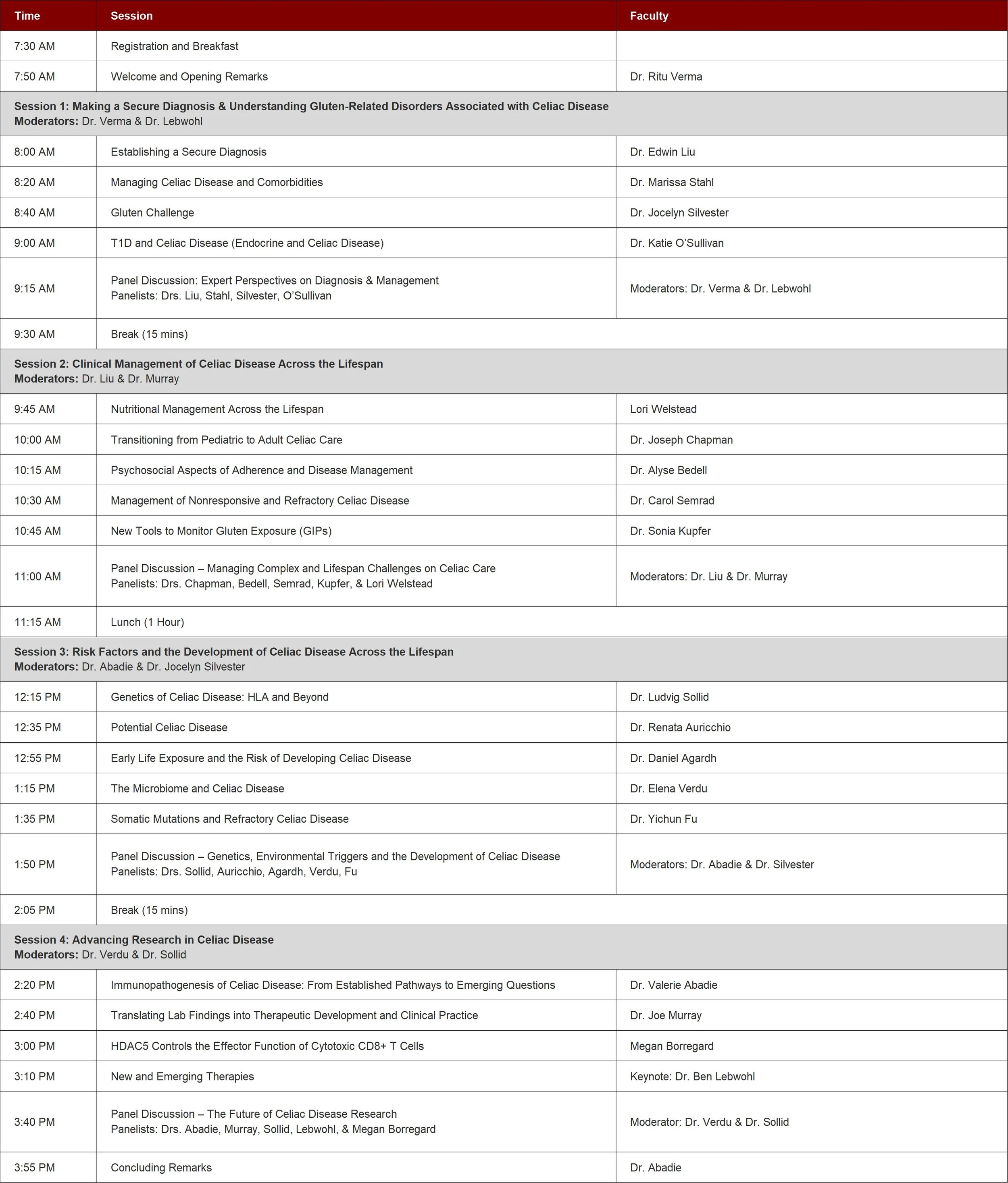
CONFERENCE AGENDA
The session recordings will be linked below after the conclusion of the conference. Then, you will be able to click the button to open the corresponding link for viewing.
Course Directors
-

Rachel Lieberman, MS
Director of Celiac Disease Center
The University of Chicago -

Ritu Verma, MD
Professor of Pediatrics
Chief, Section of Pediatric Gastroenterology, Hepatology, and Nutrition
Medical Director, Celiac Disease Center
The University of Chicago -

Valérie Abadie, PhD
Research Associate Professor
Department of Medicine,
Section of Gastroenterology,
Hepatology, and Nutrition
Committee on Immunology
Associate Scientific Director,
Celiac Disease Center
The University of Chicago
MEET THE SPEAKERS
Faculty
-

Daniel Agardh, MD, PhD
Research Team Manager and Senior Lecturer
at the Celiac Disease and Diabetes Unit Lund University, Sweden -

Renata Auricchio, MD, PhD
Associate Professor in Pediatrics
Director of Inter-Universitary Center
European Laboratory for the Investigation of Food Induced Disease (ELFID)
Head of Regional Celiac Disease Center for Children
University Federico II, Naples, Italy -

Alyse Bedell, PhD
Assistant Professor of Adult Psychiatry
Director of the Psychogastroenterology Program
The University of Chicago -

Megan Borregard, PhD
Postdoctoral Fellow
The University of Chicago -

Joseph Chapman, MD
Assistant Professor of Pediatrics
Department of Medicine
Section of Pediatric Gastroenterology,
Hepatology, and Nutrition
The University of Chicago -

Yichun Fu, MD
Assistant Professor of Medicine
Department of Medicine
Section of Gastroenterology, Hepatology, and Nutrition
The University of Chicago -

Sonia Kupfer, MD
Professor of Medicine
Department of Medicine
Section of Gastroenterology, Hepatology, and Nutrition Co-Director, Comprehensive Cancer
Risk and Prevention Clinic
Director, Gastrointestinal Cancer
Risk and Prevention Clinic
The University of Chicago -

Benjamin Lebwohl, MD
Associate Professor of Medicine and Epidemiology
Columbia University
Director of Clinical Research,
Columbia University Celiac Center, New York -

Edwin Liu, MD
Taplin Endowed Chair for Celiac Disease
Professor of Pediatrics
Director, Colorado Center for Celiac Disease
University of Colorado -

Joseph Murray, MD
Professor of Medicine,
Division of Gastroenterology and Hepatology
John and Shirley Berry
Professor of Gastrointestinal Sciences
Mayo Clinic, Rochester -

Katie O'Sullivan, MD
Assistant Professor of Medicine
The University of Chicago -

Carol Semrad, MD
Gastroenterologist and Professor of Medicine
University of Chicago Medical Center
Member of the medical leadership team
University of Chicago Celiac Disease Center -

Jocelyn Silvester, MD, PhD
Assistant Professor of Pediatrics
Harvard Medical School
Co-Director, Celiac Disease Program
Boston Children’s Hospital -

Ludvig Sollid, MD, PhD
Professor of Medicine
University of Oslo, Norway -

Marisa Stahl, M.D
Assistant Professor of Pediatrics,
Gastroenterology, Hepatology
University of Colorado -

Elena Verdu, MD, PhD
Professor, Department of Medicine
Director, Farncombe Family Digestive
Health Research Institute
McMaster University, Canada -

Lori Welstead, MS, RD, LDN
Dietitian
The University of Chicago Medicine
CME INFORMATION
Target Audience
This activity is designed healthcare professionals including physicians, basic scientists, healthcare professionals, registered dietitians and others who are interested in learning more about celiac disease diagnosis, management, care, research updates, emerging diagnostic tools and therapies.
Goals
Celiac disease is a complex, multifactorial intestinal disorder that occurs in genetically susceptible individuals following the ingestion of gluten, a protein found in certain cereals. It can manifest at any age, from infancy to late adulthood, raising important questions about its triggers and diverse clinical presentations. Since a strict gluten-free diet remains the only effective treatment, ongoing research is focused on deepening our understanding of the disease, enhancing diagnostic methods and disease management, and ultimately developing a cure.
This activity will convene leading national and international experts to explore the diagnosis, management, and research advancements in celiac disease across the lifespan, from childhood through adulthood.
This full-day symposium will cover essential topics, including:
Secure diagnosis and emerging diagnostic tools (including gluten challenge and noninvasive biomarkers)
Risk factors and screening protocols, including genetic and environmental contributors
Long-term patient management, follow-up care, and transitions from pediatric to adult care
Dietary guidance and nutritional monitoring
Psychosocial and behavioral aspects of living with celiac disease
Complex cases, misdiagnosis, and refractory celiac disease
The program is designed to benefit both clinical and research-focused audiences. Participants will gain essential updates on celiac disease diagnosis and management across the lifespan. Leading experts will present the latest breakthroughs in research and emerging therapeutic approaches.
Learning Objectives
After this activity, participants will be able to:
Explain the immunopathogenic mechanisms underlying celiac disease and their relevance to clinical manifestations.
Analyze genetic and environmental risk factors contributing to celiac disease development and their implications for population screening.
Apply current diagnostic guidelines and recommendations to establish a secure diagnosis of celiac disease across pediatric and adult populations.
Integrate multidisciplinary approaches to nutritional, psychological, and transitional care for patients with celiac disease across the lifespan.
Evaluate recent advances in noninvasive monitoring tools for gluten exposure and their application in clinical practice.
Appraise emerging therapies and research developments in celiac disease, including mechanisms of action and potential clinical applications.
Outcomes
Participation in this symposium is expected to lead to:
Improved knowledge of current diagnostic standards, serologic testing, and biopsy interpretation for both pediatric and adult patients.
Enhanced competence in designing comprehensive, patient-centered management plans that integrate nutritional, psychological, and behavioral support for all ages.
Greater ability to monitor disease progression and adherence through noninvasive testing and clinical follow-up.
Increased awareness of genetic and environmental risk factors and their implications for screening and prevention.
Broader understanding of emerging therapies and research developments that may alter the future management of celiac disease.
Collectively, these outcomes will contribute to earlier and more accurate diagnosis, optimized multidisciplinary care, and improved quality of life for patients living with celiac disease.
Practice Gaps and Needs Assessment
Despite the increased recognition of celiac disease as a prevalent autoimmune disorder, significant gaps persist in its diagnosis, management, and long-term care across the lifespan. Many clinicians remain uncertain about how to interpret serologic and histologic findings, apply gluten challenge protocols, or use emerging noninvasive biomarkers.
Furthermore, management after diagnosis often lacks standardization. Nutritional counseling and psychological support are not routinely integrated into patient care, and transitions from pediatric to adult care are frequently fragmented. Patients commonly report persistent symptoms despite adherence to a gluten-free diet, reflecting gaps in monitoring gluten exposure and addressing complex cases.
Despite advances in understanding genetic and environmental risk factors, immune mechanisms, and experimental therapies, translating basic research into clinical practice and drug development remains limited. As a result, healthcare professionals may be unprepared to identify at-risk populations, optimize follow-up care, or counsel patients on emerging treatment options.
To close these gaps, clinicians, researchers, and other healthcare professionals need up-to-date, evidence-based education on the current understanding, diagnosis and management of celiac disease. Educational needs include:
Knowledge needs: Understanding and applying updated diagnostic criteria and guidelines; interpreting new serologic and histologic markers; recognizing atypical or extraintestinal manifestations.
Competence needs: Integrating multidisciplinary approaches that include nutrition, gastroenterology, psychology, and primary care to ensure continuity and comprehensive management across life stages.
Performance needs: Implementing effective monitoring strategies to evaluate dietary adherence, detect inadvertent gluten exposure, and manage refractory celiac disease; ensuring seamless transition between pediatric and adult care; and incorporating psychosocial and behavioral interventions into care plans.
Research translation needs: Staying current with advances in immunopathogenesis, genetics, environmental triggers, and clinical trials of emerging therapies to inform future patient management and counseling.
Accreditation & Credit Designation Statement
Physician Credit
The University of Chicago Pritzker School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The University of Chicago Pritzker School of Medicine designates this live activity for a maximum of 6.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Credit
University of Chicago Medicine is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
Participants who successfully complete the entire activity and complete an evaluation form will earn 6.5 contact hours.
American Board of Internal Medicine MOC Part II Credit
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 6.5 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Other Participant Credit
Other participants will receive a Certificate of Participation. For information on the applicability and acceptance of Certificates of Participation for educational activities certified for AMA PRA Category 1 Credit™ from organizations accredited by the ACCME, please consult your professional licensing board.
Please note: The credit-claiming process will close 30 days after the activity ends. Requests to claim credit after 30 days may incur additional fees.